The Feinstein Institutes—the research institutes of Northwell Health, New York’s largest health care provider—is home to 50 research labs, 3,000 clinical research studies and 5,000 people raising the standard of medical innovation. We make breakthroughs in molecular medicine, genetics, cancer, brain research, mental health, autoimmunity and bioelectronic medicine.
Insights
5 notable Northwell advances of 2024

From the impact of sex and gender on early brain development to new treatments for a fatal lung disease, Feinstein Institutes researchers made groundbreaking discoveries in 2024
Scientists at the Feinstein Institutes for Medical Research achieved remarkable breakthroughs in 2024. Many also made headlines for advancing the research around areas like Alzheimer's care, lung disease, mental health and dysphagia. One researcher even explored how ancient viruses lurking in our DNA may influence the risk for psychiatric disorders.
These five advances showcase the power of innovative research to unlock the mysteries of human health and offer new hope for those suffering from devastating illnesses.
Here are the top five advances of 2024 from the Feinstein Institutes.
The dark side of genetics and psychiatric disorders
Up until recently, 98-99% of the human genome was considered “junk DNA.”
Also known as the "dark genome," this massive portion of our genetic blueprint was thought to be irrelevant to our biology because it doesn't produce proteins — which are essential for life and allow our bodies to function properly. However, emerging research is proving this “junk” is active and could be influencing our mental health.
A team led by Douglas Nixon, MD, PhD, director of the Institute of Translational Research, discovered a potential link between this “dark genome” and the risk of developing conditions like schizophrenia, bipolar and major depressive disorder.
Their research focused on human endogenous retroviruses (HERVs), which have been embedded in our DNA for millions of years. Like a recipe ingredient that you can’t taste, see or smell, HERVs are present but mostly dormant — or so we thought.
“I was shocked to find that 9% of everyone’s genome is actually the remnants of ancient infectious viruses, not so dissimilar to HIV,” Dr. Nixon said. “Retroviruses have been infecting us and our ancestors throughout human history, and very few people have actually been studying what these might do.”
While some scientists have theorized that HERV activity in psychiatric patients might be linked to immune responses and inflammation from infections, this new research suggests a different mechanism and a potential direct link to these disorders. Published in 2024 and recognized as the Gershon Paper of the Year by the International Society of Psychiatric Genetics, the study found that variations in inherited HERVs may influence an individual's risk for these psychiatric conditions.
“For the first time, we’re now able to think about psychiatry through the lens of biology and the genetics buried in the dark genome,” Dr. Nixon said.
More than 4,500 HERVs were found to be expressed in the brain. While most weren't individually linked to specific disorders in this study, several were found to be associated with:
- Schizophrenia risk
- Both schizophrenia and bipolar disorder
- Major depressive disorder
Dr. Nixon’s research was partly funded by the United Kingdom National Institute for Health and Care Research (NIHR) and the United States National Institutes of Health (NIH).
While genetics is just one piece of a complex puzzle when it comes to evaluating risk for these psychiatric disorders, Dr. Nixon’s team believes this discovery could pave the way for better diagnostic tools.
What’s next?
The team is now investigating whether these HERVs produce proteins — something that other research has proven possible for some dark genome proteins. If HERVs are among them, this could help develop a blood test to detect risk for psychiatric disorders. “We want to be able to provide treatments for people who’ve already been diagnosed, as well as help to slow or prevent major psychiatric diseases like schizophrenia,” Dr. Nixon said. “I’m hoping that the work we’ve done will lead to new treatment options in the future.”
Beyond the binary: gender's broad impact on brain function
A new study offers biological evidence that sex and gender are, in fact, distinct. Recognizing this can, study author Elvisha Dhamala, PhD, said, improve the quality of research and how people are treated medically.
“Everyone has a gender, and these findings are relevant to all individuals, not just those identifying as nonbinary or gender fluid.”
Dr. Dhamala, a computational neuroscientist, analyzed brain imaging data along with self- and parent-reported gender information of nearly 5,000 children aged 9 and 10 and found that sex and gender influenced brain activity in distinct ways. The data, taken from the Adolescent Brain Cognitive Development (ABCD) study, was collected at 21 different sites across the U.S. Using machine learning, the researchers compared how sex and gender map onto functional brain networks, which are comprised of brain regions that communicate with each other and work together to produce function.
Here are the definitions researchers used for each term and the impact each were found to have on the brain:
- Sex is assigned at birth as either male, female, or intersex, although only binary male and female sex were considered in this study.
- Results: In the study, sex was found to influence brain regions associated with visual and sensory processing, motor control, and executive function.
- Gender was considered along a continuum encompassing identity, expression, and other related factors.
- Results: The research found that gender showed a more dispersed influence across the brain, impacting areas involved in executive function, attention, social cognition, and emotional processing.
This suggests that while sex has a more localized impact, gender's influence is broader.
“In the last decade, there has been a lot of emphasis to try and understand how sex differences might make men or women more vulnerable to specific illnesses as a way to better tailor treatments,” said Dr. Dhamala, who is also assistant professor of psychiatry at the Feinstein Institutes and Zucker Hillside Hospital. “We must also account for gender as distinct from sex when conducting trials — not just in terms of who we’re studying but also who is actually doing the research. It will lead us to have a lot more perspective on the types of research questions we should be asking and the types of things that matter for health and wellness.”
While not a common practice currently, Dr. Dhamala emphasized its importance going forward. “Conflating sex and gender hinders a nuanced understanding of their separate influences on health and behavior.”
What’s next?
The NIH-funded ABCD study will follow nearly 12,000 children over ten years, exploring brain development and child health in the U.S. This will allow researchers like Dr. Dhamala, who is not a part of that study, to track how participants evolve during adolescence and beyond.
“We’re now really excited to look at how sex and gender and the ways in which they map onto the brain might actually change over time throughout the course of development,” Dr. Dhamala said.
Rethinking thick liquid diets
Could a common treatment for swallowing difficulties in people with dementia actually be doing more harm than good? New research from the Feinstein Institutes is challenging the long-held belief that thickened liquids protect against health risks like pneumonia.
For years, these modified drinks, which resemble baby food consistency and honey or cough syrup thickness, have been the go-to solution for people with dementia who struggle to swallow, a condition known as dysphagia. This condition affects about one-third of older adults and 90% of those hospitalized with dementia.
Thin liquids come in fast and, instead of moving from the back of our throat (pharynx) into the esophagus and stomach, these patients run the risk of having it go down the airway — more commonly referred to as “going down the wrong pipe.”
“This can cause choking or aspiration pneumonia, which could be dangerous among older adults and frightening for caregivers,” said Liron Sinvani, MD, author of the paper. “If you thicken the fluid, it moves slower and patients are better able to avoid these hazards and swallow with more confidence.”
Listening to the complaints from her own patients about this dysphagia diet, the geriatrician searched the literature for evidence supporting this practice. “We found that there was none.”
Dr. Sinvani and her co-author, Alex Makhnevich, MD, analyzed medical records of nearly 9,000 patients and found no difference in survival rates between those who received thickened liquids and those who didn't. Their research also revealed that patients on thickened liquids were more prone to other respiratory problems. “The bottom line from our study is to show that things may not be as clear-cut as we think,” Dr. Sinvani says.
“There are probably patients that would benefit from thickened liquids and dysphagia diets, but there are probably patients that don't, where the impact on quality of life overtakes the benefit. This universal practice that impacts quality of life needs to be further investigated.”
What's next?
Dr. Sinvani's team is working on exciting new research, including a project using artificial intelligence to predict which patients could have dysphagia improvement and benefit from a less restricted diet. They're also developing a website called "We Care to Feed Dysphagia" to provide much-needed information and support for caregivers.
Recognizing psychosis in Alzheimer's patients
Imagine a disease that robs your memories and your grasp of reality. For a staggering 40-50% of Alzheimer's patients, this nightmare is a reality. Psychosis, characterized by delusions and hallucinations, adds another layer of complexity and distress to an already devastating illness.
But what if doctors could predict and potentially intervene before these harrowing symptoms take hold?
A groundbreaking 2024 study from the Feinstein Institutes for Medical Research offers a glimmer of hope. Their results point toward the potential for a simple blood test to detect psychosis in Alzheimer's patients. “We focused on a protein called tau, which is known to accumulate in the brains of individuals with Alzheimer's,” said Jeremy L. Koppel, MD, a geriatric psychiatrist, associate professor at the Feinstein Institutes’ Institute of Molecular Medicine, and co-lead author on the study. “More specifically, we examined a modified form of tau called phosphorylated tau (ptau), known to be a hallmark of brain tangles in Alzheimer’s disease and found in the brain in soluble forms that then circulate into the blood and the periphery where it can be measured.”
Having previously studied brain tissue samples of deceased donors, and PET imaging for tau proteins in the brain, in this study Dr. Koppel analyzed blood biomarkers and clinical data taken from a group of close to 1,000 living participants. “When we talk about blood biomarkers in Alzheimer’s disease, we’re really talking about a constellation of proteins that together with clinical information can be used to make a pathology-based diagnosis with a high degree of certainty even in the absence of a biopsy or a postmortem examination.”
In their study, Dr. Koppel and co-author on the paper Jesus J. Gomar, PhD, found that individuals who later developed psychosis showed a distinct pattern: their blood levels of p-tau rose before any signs of psychosis appeared. These levels peaked around the time psychosis emerged and then declined, although they remained elevated compared to those without psychosis.
What’s next?
This discovery opens exciting possibilities. By measuring p-tau levels in the blood, doctors may one day be able to identify individuals with Alzheimer’s disease at risk of developing psychosis. It may even help to diagnose those who are very impaired and experiencing psychotic symptoms that are communicated only in aggressive behavior, paving the way for earlier interventions and support. “While more research is needed before this blood test becomes a standard diagnostic tool, it represents a significant advance in our understanding and management of this challenging aspect of Alzheimer's disease.”
He added that these proteins also have the potential to become viable targets for safe and effective therapies, even in patients who have difficulty communicating — a huge advance over what is available now.
Researchers focus on the spleen to treat the lungs
Pulmonary arterial hypertension (PAH) is a debilitating and often fatal lung disease. Current treatments offer little hope: They help manage symptoms but can’t address the underlying cause. Now research suggests that a key to managing PAH may not be in the lung, but in another organ entirely.
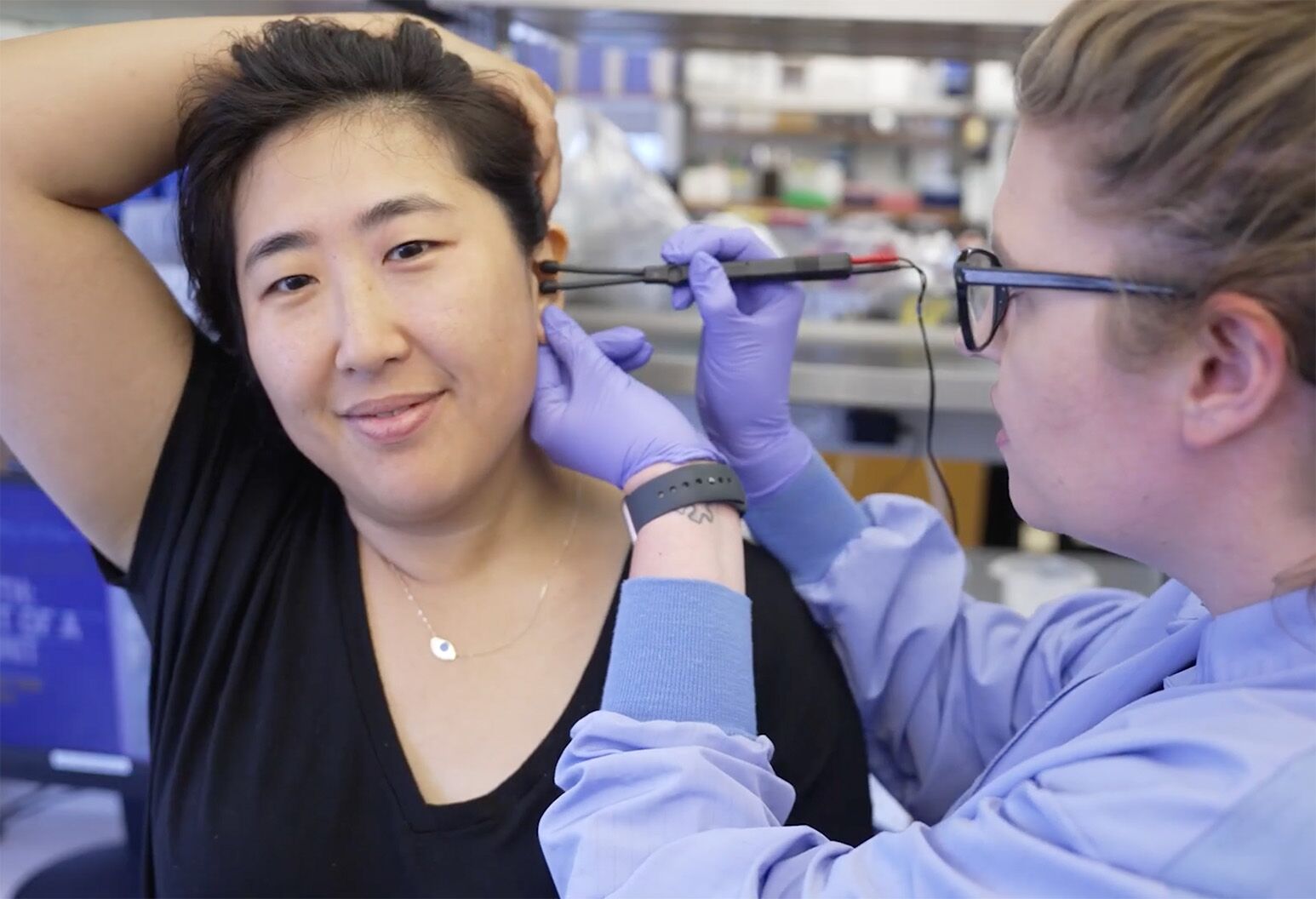
Researchers at the Feinstein Institutes for Medical Research are exploring an experimental, noninvasive therapy that targets the spleen, a key player in the immune system. An approach known as focused ultrasound may provide a solution.
Unlike existing medications that temporarily reduce blood pressure in the lungs, focused ultrasound aims to quell the inflammation that drives the disease. “Within the spleen lies the splenic nerve, a crucial player in regulating the immune response,” said Stavros Zanos, MD, PhD, senior author of the study. “The focused ultrasound device is placed on the patient's abdomen, and using image guidance, the sound waves are precisely targeted at the spleen and the splenic nerve.”
These high-frequency sound waves, while inaudible to the human ear, generate mechanical vibrations that activate the splenic nerve, which in turn communicates with the immune system to reduce the chronic inflammatory response. “We don’t yet know why, but this appears to have a ripple effect throughout the body, ultimately reducing inflammation in the lungs and improving the function of blood vessels in the lung and of the heart,” Dr. Zanos said. “We are currently studying this newly established spleen-lung communication and exploring how to translate these findings into clinically viable therapies”.
In preclinical studies in rats, this targeted ultrasound approach significantly reduced lung pressure and improved heart function. Importantly, the benefits persisted even after the treatment was stopped, suggesting the potential for long-lasting disease modification.
What’s next?
Researchers are now working to translate these findings into clinical trials for humans, particularly focusing on the younger women predominantly affected by this devastating disease.
This research not only offers a potential new treatment for PAH but also sheds light on the disease's underlying mechanisms, highlighting the critical role of inflammation in chronic cardiovascular diseases.