The Feinstein Institutes—the research institutes of Northwell Health, New York’s largest health care provider—is home to 50 research labs, 3,000 clinical research studies and 5,000 people raising the standard of medical innovation. We make breakthroughs in molecular medicine, genetics, cancer, brain research, mental health, autoimmunity and bioelectronic medicine.
Insights
Vagus nerve stimulation: What experts need you to know
More than half of all deaths worldwide are linked to chronic inflammation. Using vagus nerve stimulation on a variety of conditions could someday change that.
Heart disease. Asthma. Colitis. You wouldn’t think they’re related, but they are. So are obesity, rheumatoid arthritis and diabetes. All these dangerous conditions have one thing in common — chronic inflammation plays a role in their development.
Here’s where things get interesting: There’s an effective, drug-free way to target chronic inflammation called vagus nerve stimulation. Researchers are finding that stimulating the vagus nerve could be key to treating all these conditions and more.
What is vagus nerve stimulation?
Vagus nerve stimulation is a medical treatment that uses devices to deliver electrical impulses to the vagus nerve, one of the longest nerves in the body. This helps control the level or intensity of inflammation in the body. Currently, it is FDA-approved as a treatment for epilepsy, treatment-resistant depression and stroke rehabilitation. And studies are underway for use with over a dozen other diseases.
To understand how vagus nerve stimulation could possibly treat so many different conditions, first you need to understand the various roles the vagus nerve plays in our bodies and its link to regulating inflammation.
What is the vagus nerve?
We have 12 nerves that run from our brains throughout our bodies; they’re known as cranial nerves. They constantly relay information between tissue, organs and other body systems and the brain.
The optic nerve, for example, is responsible for our vision; the olfactory nerve extends to the nose to relate messages regarding scents.
The largest and longest of these nerves is known as the vagus nerve, which gets its name from the Latin term “vagary”, which means wandering. The vagus nerve consists of two major bundles, one on either side of our neck; combined, they contain more than 200,000 individual fibers.
In all, the vagus nerve travels more than a foot and a half from the stem of the brain to the heart, lungs, stomach, pancreas, digestive tract, kidneys, spleen and liver, among other places. This cranial nerve is responsible for a host of vital duties, such as regulating heart rate, breathing and blood pressure; it’s also a vital part of the immune system.
Podcast transcript — Vagus nerve stimulation pioneers talk RESET-RA trial and the promise of this revolutionary treatment
The vagus nerve and inflammation
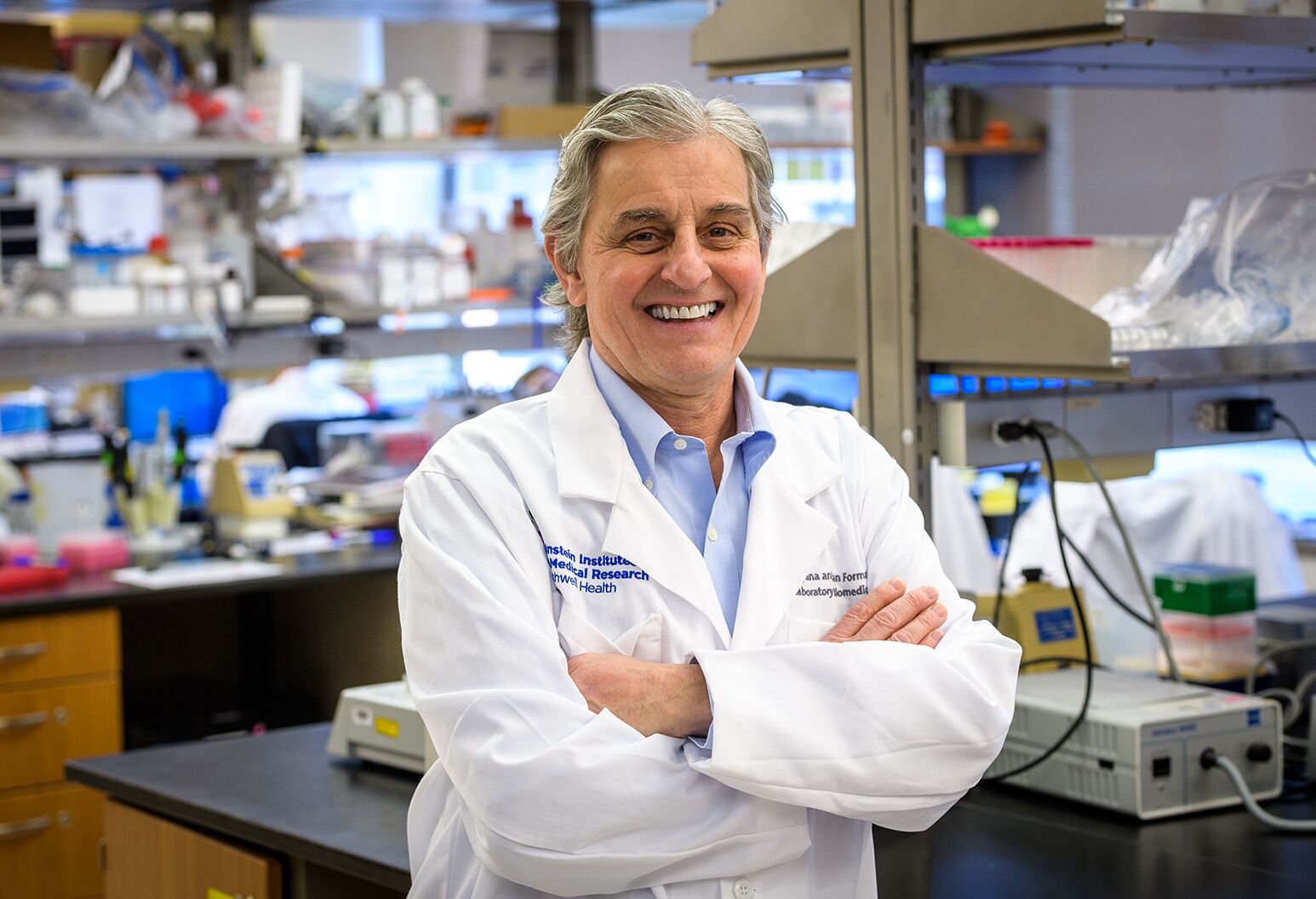
Nearly a quarter of a century ago, Kevin Tracey, MD, president and CEO of the Feinstein Institutes for Medical Research, first described how the vagus nerve regulates small proteins called cytokines that aid in the inflammatory response. He found that whenever diseases or injuries are detected, the vagus nerve signals the body and the brain to initiate a defense mechanism, sending these inflammatory cells to the site of the problem to begin the healing process.
But the vagus nerve can also be the source of more serious problems when it’s not working properly. That’s when chronic inflammation — where the body releases inflammatory cells into your system, even when there is no longer injury or threat of disease — can occur and where vagus nerve stimulation could help.
“The earliest experiments of using vagus nerve stimulation in the lab revealed that a small amount of current on the vagus nerve reduced the amount of cytokines,” Dr. Tracey said. “It is like stepping on the brakes in your car. You can slow down the amount of inflammation for patients with chronic inflammatory conditions.”
This finding gave rise to vagus nerve stimulation, said Dr. Tracey, along with a class of medications known as biologics. While these drugs — made from living cells or organisms — have become an important method for treating inflammatory conditions, Dr. Tracey notes, they are not the final answer. “These biologics have side effects. They are very expensive and they have to be injected, and they only work in about 40 or 50% of patients,” he said. “My colleagues and I were looking for an alternative way to treat inflammation and stop cytokines.”
The stakes are high. Diseases associated with or made worse by chronic inflammation account for 40 million of the 60 million deaths worldwide each year. “We’re talking about heart disease and stroke, sepsis, cancer and diabetes, to name a few,” Dr. Tracey said.
He notes that inflammation is also a contributing factor in mental health issues like depression and chemical dependency, as well as neurodegenerative diseases like Alzheimer’s and Parkinson's.
While these diseases each have their own intricacies and manifest their symptoms uniquely, they all have at least two things in common: chronic inflammation and a malfunctioning vagus nerve.
Vagus nerve reset
While scientists are still working to map the vagus nerve in its entirety, research has revealed some promising information. Studies in the lab have shown that when the vagus nerve is severed in mice, the immune system begins releasing a continuous stream of inflammation-related cells into the body that damage otherwise healthy cells. This is similar to the process in humans that leads to autoimmune diseases like epilepsy, Crohn’s and multiple sclerosis.
Conversely, researchers have found that if they interrupt that process by stimulating the vagus nerve, it can help to recalibrate the immune response and more normally regulate the amount of inflammatory cells released into the body. “Our research was the first to indicate that we're very close to a time when millions of patients will benefit from vagus nerve stimulation for the treatment of a wide variety of diseases,” Dr. Tracey said. “It’s very exciting.”
How to stimulate the vagus nerve
There are many ways to stimulate the vagus nerve, though some are more effective than others. Spend much time on the internet and you’ll quickly come across fads promising to “reset the nervous system” with everything from cold water ice baths to Tai Chi to vagus nerve exercises.
The truth is the vagus nerve can benefit from simple, everyday activities. Exercise, meditation and even humming all are associated with a slower heart rate, which Dr. Tracey explained may improve vagus nerve function. “The mechanisms of action that would be relevant to these self-help strategies are still not well understood. But it is certainly interesting enough to study further,” he said.
Here’s what researchers do know: A growing body of research has shown that, as a medical intervention, stimulating the vagus nerve has promise as an effective, drug-free treatment.
Vagus nerve stimulation devices
Vagus nerve stimulation is one exciting example of bioelectronic medicine, a new field that uses devices, rather than medications, to treat disease. The idea is to sidestep the side effects (and costs) that often come with medications like biologics and offer a new path for patients living with chronic and potentially life-threatening diseases.
Decades of research have produced different approaches to vagus nerve stimulation, and they can be broken into two categories: direct and indirect.
Indirect vagus nerve stimulation
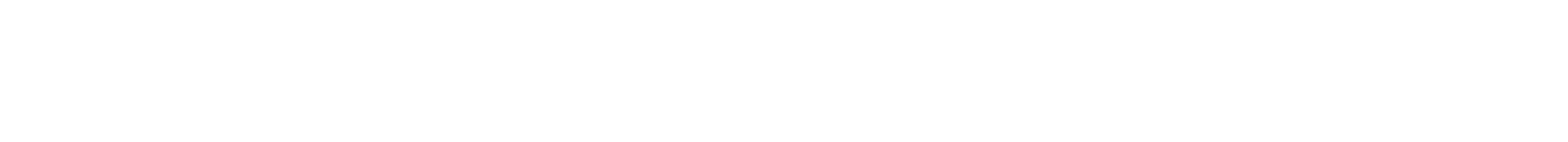
Transcutaneous vagus nerve stimulation (t-VNS)
This is a non-invasive approach that uses a stimulation device attached to different parts of the ear. In Europe, this method has been approved to treat epilepsy, chronic pain and depression. In the U.S., the FDA has approved it only for cluster headaches, but research is ongoing into a number of autoimmune diseases and conditions, including recent work on inflammatory bowel disease in children.
Transcutaneous electrical nerve stimulation (TENS)
As opposed to affixing a stimulator to the ear, this approach uses small electrode pads (sometimes referred to as a TENS unit or TENS device) placed in specific areas of the body to stimulate different areas of the vagus nerve. A TENS unit is commercially available and has a range of applications. Researchers at the Feinstein Institutes have launched initial studies to see if patients can use small, wearable TENS units throughout the day to stimulate the vagus nerve and someday treat conditions like diabetes or to help patients lose weight without diet drugs.
Ultrasound stimulation
An ultrasound is commonly known as a noninvasive imaging test, but it can also be used for therapeutic purposes, as it’s another method to target specific portions of the vagus nerve and reduce inflammation in the body. A first-in-humans study led by researchers at the Feinstein Institutes, Sangeeta S. Chavan, PhD, and Stavros Zanos, MD, PhD, and GE Research found spleen-focused ultrasound stimulation (FUS) lowers levels of endotoxin-induced tumor necrosis factor (TNF) in the body, which is an inflammatory protein. Ultrasound therapy has also been shown to reverse diabetes and reduce obesity in preclinical trials.
Direct vagus nerve stimulation
Implanted vagus nerve stimulation device (VNS)
This approach involves implanting a pulse generator under the skin in the chest and attaching a small, vitamin-sized device directly on the left vagus nerve, particularly because the vagus nerve on the right side of the body is more likely to affect the heart. The implantation takes about one to two hours, and patients can usually go home in one to two days.
The implanted vagus nerve stimulation device sends a 30-second electrical pulse to your vagus nerve every five minutes. “We know that if you put electric current in pulses for short periods of time directly onto the vagus nerve, you can control inflammation through the inflammatory reflex in animals and people,” Dr. Tracey said. The devices are built with batteries that can last eight to 10 years but can be turned off or modified by doctors as needed.
Approved uses
Vagus nerve stimulation for epilepsy
The first implanted vagus nerve stimulation device was approved by the FDA in 1997 to treat epilepsy in patients 12 years and older. In 2022, new guidelines expanded the patient pool to include patients as young as four. This treatment is available for patients who have focal (partial) seizures, don’t qualify for or have access to epilepsy surgery, and continue to experience frequent seizures despite trying anti-seizure medications.
Patients typically see the full effects of this VNS therapy one month to a year after surgery and it’s most effective when combined with medication, studies show. Patients are given a magnet to manually trigger the device in the event of a seizure to help shorten or reduce the severity of the episode. About half of patients report a reduction in seizure frequency by at least 50% after one to two years. Some also report improved mood, cognitive function and overall well-being.
Vagus nerve stimulation for depression
In 2005, the FDA approved vagus nerve stimulation devices for patients with treatment-resistant depression. This includes patients who have had major depressive disorder (MDD) or have not responded well to antidepressant medications and therapy, electroconvulsive therapy (ECT), or transcranial magnetic stimulation.
Unlike epilepsy treatment, vagus nerve stimulation for depression runs continuously, with pre-set intervals rather than manual activation. Studies have found that 30% to 40% of patients report a significant reduction in depressive symptoms after one year, and 20% to 25% experience an extended period free from significant depression. Those who benefit report better mood stability, energy, and overall quality of life.
Vagus nerve stimulation is intended to be used alongside other forms of treatment, such as medications or psychotherapy. Like antidepressant medications, it may take several months or even up to a year for patients to experience the full benefits.
Vagus nerve stimulation for stroke
In 2021, the FDA approved vagus nerve stimulation as a treatment for stroke rehabilitation, particularly for those who continue to experience residual weakness or limited mobility in their arms and hands. During stroke rehabilitation, the therapist triggers the device to stimulate the vagus nerve whenever the patient performs a specific movement or exercise — a technique called "paired stimulation".
After about six weeks of VNS-paired therapy, studies have shown that about 47% of patients achieved clinically meaningful improvements in their arm strength and function and two to three times greater improvement in arm and hand function compared to those who received physical therapy alone. These improvements were sustained for months after the initial treatment, the studies showed.
Potential future applications
Research continues on a host of other conditions. Those include:
- Alzheimer’s disease and dementia
- Anxiety disorders and PTSD
- Crohn’s Disease
- Diabetes
- Fibromyalgia
- Heart failure
- Inflammatory bowel disease (IBD) in children
- Long Covid and post-infectious syndrome
- Kidney diseases
- Migraine and cluster headaches
- Multiple sclerosis (MS)
- Obesity and weight management
- Parkinson’s disease
- Rheumatoid arthritis
- Sepsis
- Sleep disorders
- Traumatic brain injury (TBI)
Many of these applications are still in early research or clinical trial stages, but the findings so far indicate that VNS could be a promising therapy across multiple fields of medicine. Leading the way on this cutting-edge research is the Feinstein Institutes at Northwell Health, which was awarded nearly $7 million by the National Institutes of Health to create the first comprehensive map of the vagus nerve.
The goal of the three-year project is to decode how each fiber in the vagus nerve affects different systems in the body — something that remains a mystery today. Like mapping which areas of the brain control different bodily functions, this will inform new techniques and help researchers tailor treatments for certain conditions or diseases.
“My colleagues and I at the Feinstein Institutes and elsewhere are pursuing the very important question of whether or not we can make devices to stimulate the vagus nerve that will not have the expense or side effects of many of the potentially dangerous drugs that patients are using today to treat their inflammatory conditions,” Dr. Tracey said.
“This is not a dreamy futuristic wish list. There is evidence that this may be possible sooner rather than later for many of these conditions and there are hundreds if not thousands of people working on these ideas.”
Vagus nerve stimulation side effects
Vagus nerve stimulation is not suitable for everyone. Patients with conditions of the heart and lungs, for example, should consult their doctor to assess suitability. Vagus nerve stimulation devices run on a battery that usually lasts five to 10 years. When the battery runs out, a minor surgical procedure is required to replace it. Device malfunctions may occur, but are rare and usually correctable.
As with any surgery, there is a risk of infection at the site where the device is implanted. Follow all post-operative instructions to reduce this risk. Pain or discomfort around the implant site can occur but typically only lasts a few days to weeks. There is a small risk of damage to the vagus nerve or surrounding tissues during the implantation.
When the device is actively stimulating the vagus nerve, patients may experience mild shortness of breath, coughing, soreness or tingling in the throat, discomfort near the location of the vagus nerve, or a change in voice quality (this may occur because the vagus nerve plays a role in vocal cord movement).
Those considering vagus nerve stimulation should also consider that this treatment does not provide immediate results. It may take several months to experience the full therapeutic effects, particularly for conditions like depression or epilepsy.
Patients may need to make certain adjustments during the early stages of treatment, such as avoiding strenuous physical activities that could be impacted by the stimulation.